Podcast: Play in new window | Download (Duration: 24:03 — 34.0MB) | Embed
Given that this episode is coming out the day after Christmas (and considering all of the feasting that often comes with this time of year!), I thought it was a timely opportunity to talk about digestion from a Chinese Medicine perspective, and to share some pearls of wisdom that have stood the test of time over millennia. Chinese Medicine has long understood, and almost revered, the role that the gut and digestion play as a foundation for all-round health of mind and body. As a result of this, in Chinese Medicine we have a whole pillar of practice that focuses on nutrition or dietary therapy, and which offers guidelines not only on what to eat, but how to eat it. Listen in to hear some simple, natural tips to boost digestion!

Show Notes
Transcript
Hi everyone and Merry Christmas, happy holidays. Given that this episode is coming out on Boxing Day (and considering all of the feasting that often comes with this time of year!), I thought it was a timely opportunity to talk about digestion from a Chinese Medicine perspective – and to share some pearls of wisdom that have stood the test of time over millennia. Chinese Medicine has long understood – and almost revered – the role that the gut and digestion play, as a foundation for all-round health of the mind and body and emotions. In many of the traditional diagrams that outline the interconnectedness of the various organs and systems in the body, the digestion (which we also refer to as the Spleen and Stomach, or the Earth, because it forms the foundation for everything) is often placed at the center of these schematics, which highlights its central and fundamental role.
And because of this in Chinese Medicine, we have a whole pillar of practice that is Chinese Medicine Nutrition or dietary therapy, which offers guidelines not only on what to eat, but also how to eat it. Also, many of our acupuncture points, and therapies like moxa (which is heat application) or infrared lamp and the herbs that we use – all of these modalities have been shown to have an impact on gut health as well, whether by raising certain bacterial populations in the gut, or by improving the efficacy of digestion.
This perspective regarding the importance of gut health is something that biomedicine has recently come around to as well, with an ever-growing body of research into the role of the microbiome and gut bacteria. The microbiome is the sum total of all of the bacteria and microbes that live in and on our bodies, so when we consider the number of cells that make up our body or what we think of as our human body, the number of bacterial cells of vastly outnumbers the human cells by a factor of roughly 10 to 1 – which might prompt some musing on what it means to be human, and what our perception of ourselves is based on, if 90% of the cells that make up our whole being are actually bacterial cells! It’s quite mind boggling, isn’t it?!
A healthy and balanced microbiome is fundamental to thriving, good health because the bacteria that live in and on us aren’t just freeloading – they actually have many important roles in the function of our body. This includes important processes, like the metabolism and assimilation of nutrients… they’re involved in immune regulation, And mood and brain regulation. Many of you might have heard the fact that 90% of serotonin, which is our happy feel good neurotransmitter, is made in the gut, so having a healthy, happy, balanced gut bacteria is truly essential to good health.
Meanwhile, an imbalanced microbiome has been linked to a whole range of symptoms and conditions from diabetes to depression, anxiety, autism, asthma, rheumatoid arthritis, multiple sclerosis, and a whole host of inflammatory bowel conditions. And that’s just the tip of the iceberg! In an attempt to rebalance the microbiome, we’re seeing all manner of interventions, from the relatively benign or simple probiotics (and probiotic foods), also prebiotic foods (which give us the substrate or the materials for the probiotics to thrive); we’re seeing antibiotic therapy in some cases where we’re just obliterating all of the gut bacteria (or all the susceptible bacteria), and we’re also seeing on the extreme end, things like fecal transplants, which is the transplant of healthy fecal matter – so healthy poos basically transplanted into the bowels of those who are affected by certain conditions. What we often find is that with the transplant of that bacteria, we’ll see an improvement and that can be maintained if the underlying foundation of gut health is looked after at the same time.
In Chinese Medicine, we are always looking to get to the root of the imbalance – to get to the foundation and correct it from there. So when looking at gut health and gut bacteria, we can take the analogy of a garden, for example. When we think about a garden, say, if it’s got poor soil or it’s marshy or it’s receiving insufficient light or drainage, we’re going to have trouble growing the healthy balance of plants – or bacteria – that we want in order to have the maximum benefit; what we might see instead is an overgrowth of weeds – which would be reflective of the non-beneficial bacteria which crowd out the space for everything else, and all the plants that we actually want to grow. One way to resolve the weeds, is to bomb everything – like a blanket-clearing of everything, as with antibiotics – just raze everything to the ground. It will be a short term fix, but it won’t necessarily fix the underlying imbalance, as once you’re done with the antibiotics, the non-desirables can often come back – and often in greater force as you’ve already damaged the soil in the garden. An example of this might be some of the experimental therapies looking at antibiotic infusions for people suffering with arthritis and other autoimmune conditions. They have ound that using antibiotics could confer short term benefits, but the long-term benefits were sketchy because, again, it was obliterating all of the gut bacteria. Similarly using probiotics or fecal transplants without addressing the underlying health of the soil or the underlying imbalance is like just planting desirable plants or bacteria into an unprepared or untended garden. They might hang on for a bit, but they won’t be able to gain a strong foothold unless the foundation is addressed. In Chinese medicine, this is a big part of what we do -we look at how we can support this essential function of digestion, which is so fundamental to life and health.
To bring up another analogy, in Chinese medicine – as in Ayurveda and other traditional age-old medicines – we view the digestion as a cooking pot, or cooking fire, and the healthier and more powerful our digestive fire, the better our assimilation of nutrients, and therefore the better our health and vitality. If the digestive fire is strong, we can break down all the food that we eat efficiently and completely, which allows us to absorb maximal nutrition. In Chinese medicine, this is why we say you are not only what you eat, but you are also what you can digest. You might be eating all the amazing superfoods, but if they’re not being absorbed completely, you’re not getting the maximum benefit from them. Another benefit of strong, efficient digestion is that food gets broken down in the appropriate point of the digestive tract. If digestion is weak, foods that should be more thoroughly broken down at the upper end of the digestive tract (around the stomach) reach the lower end (the intestines) insufficiently digested, and there they can cause improper fermentation, which might manifest as bloating, gas, and irritation of the gut lining. And this irritation of the gut lining is another concern, because over time when that delicate gut lining is being continually aggravated, it can contribute to a situation of leaky gut, which is where the cell junctions (of the cells lining the wall of the intestines) become looser, and allow the materials from inside the digestive tract to permeate into the body. Now the digestive tract is meant to be a sealed closed system, so when matter leaves here and leaks out of the gut into the systemic circulation, it is rightfully picked up by the body as foreign – it’s “not-self”. This can trigger a whole host of immune and autoimmune reactions such as joint pains, mucus production, lethargy, mood swings – a whole host of symptoms. And we’ll get more into this in future episodes as well, and particularly the role that gluten that is sprayed with certain substances can play in this.
So that explains why complete digestion – and a healthy digestive fire is so essential to our health. One of the ways that we maintain the strength of our digestive fire, and keep stoking it, in Chinese Medicine is with warm and cooked food, and warm drinks as well. And I do get a lot of eye rolls from patients when I first bring this up, especially in summer, when people say, “Oh my God, but it’s hot. What am I going to eat?” This is where we can look to a lot of the Southeast Asian cuisines, and Indian cuisines, for inspiration – or even Middle Eastern: these are all hot climates and yet we don’t see a proliferation of raw food. In fact, we see a strong focus on warm food and alsodigestive herbs and spices, like ginger or pepper for example, that help to support digestion. Also in a lot of these climates, we see people reaching for warm drinks: for example, in Hong Kong, I love how they have the hot water dispensers available in the airport and public spaces, and I love that we’re seeing these pop up at the Gold Coast picnic areas! This is awesome, and such a great way to look after our guts when we’re on the move. So yes, in a lot of those warmer climates, we actually see that people are consciously reaching for warmer food and drinks. This is so important for the gut because when we look at the stomach, it is layers and layers of muscle and we know that in order for muscle to function efficiently, it needs to be warm and supple. So throwing cold stuff into our stomach is like literally icing those muscles, and stopping them from doing their work efficiently. This can be a real issue because the stomach wall, which is lined with layers of muscles, also releases a lot of factors that are essential for our digestion. It releases stomach acid, it releases pepsin (which is a enzyme that breaks down proteins) and it releases a substance called intrinsic factor, which is essential to B12 assimilation in the body as well. All of these things are so essential to our digestion, so we want our stomach to be nice and warm and supple. Many of us might have had a direct experience of how much the stomach doesn’t like being cold, and that is the “ice cream headache”. When we throw something cold in the stomach, the stomach cramps up – and interestingly the Stomach channel pathway, or the connective tissue pathway that links the stomach to other parts of the body, travels up to the center of the forehead, which is exactly where those ice cream headaches hit us. That’s a very clear example of how the stomach likes to be kept warm, and if something doesn’t feel good, that’s always a good indicator that something’s off.
With respect to the warm and cooked food as well, I always suggest to people to look at what has stood the test of time – what kind of eating has worked for people in traditional cultures over millennia? We’re seeing a bit of a trend in raw food at the moment, but at the same time I’m also seeing patients in clinic with all sorts of digestive issues, irregular bowel movements, bloating, fatigue, headaches, brain fog and so on – and often when we switch to the warm and cooked foods (together with other treatments), people are amazed at the difference that they feel. I think it’s also important to consider that we are not ruminant animals. Unlike animals, like cows and sheep and giraffes, that eat large amounts of raw vegetable matter – these guys have been blessed with multiple stomachs, which gives their body ample time to break down the plant fibers that are harder for us to digest. We developed as we did in large part thanks to the discovery of cooking fire, because cooking food allowed us to unlock greater stores of energy and allowed us to make many more nutrients more bioavailable, and easier for us to digest. Raw food might feel good for a little, while the digestive fire still has some remnant energy. But over time, generally I find that it can lead to various imbalances – I go into a little bit more detail on this in one of my blog posts on my website, and I also have a whole lot of recipes that have more of a warm and cooked focus – and also, just in time for summer, some healthy cooked salad options! Eating warm and cooked foods doesn’t mean you miss out on salads. Veggies are amazing! We should all be making them a large focus of our diet, but there’s ways to make these summer salads more digestion friendly, so check out that post as well.
In the same way that warm food is going to keep our digestion firing on all cylinders, so will the drinks that we drink. Choosing warm drinks, like herbal teas – or for extra digestive power, you can throw some fresh ginger, (which is a digestive stimulant) in a cup with some boiling water, you can add lemon (which is another digestive stimulant), and even a pinch of salt, which will not only help with rehydration in the current hot summer that we’re having in Australia, but it also can be a precursor for the hydrochloric acid production in the stomach, so it’s an all-round digestive booster.
Another big thing we can do to support our digestion, and ensure complete function, and beat any bloating and fermentation and gas, is to chew our food well. Saliva contains an enzyme called amylase – this is an enzyme which breaks down starches, and in fact it does about 30% of the starch digestion. This is why it’s really important not to skimp on this step. Make sure you chew your food well! Get that saliva mixed through, let that amylase start to kick off that digestive process.
Another factor to consider if you are experiencing some digestive difficulties, or any bloating or fatigue after meals, brain fog and so on, is to limit sugar – and by this I also do mean natural sugar. Sugar is sugar! And if you’re experiencing any of the symptoms that I just mentioned, then giving any potential non-beneficial bacteria that might be living in your gut, giving those guys less easy fuel (less sugar) can starve them off, and allow beneficial bacteria more space to thrive. In Chinese Medicine, fruit doesn’t have such a starring role as it does in our modern diet. I think it’s interesting to consider the sugar content of many smoothies out there, and fruit juices – it’s equivalent to a can of Coke, or a Snickers bar. So even though it’s coming from nature, it’s still having similar effects in the body – it’s still spiking our blood sugar, and derailing hormones, and potentially knocking gut bacteria out of balance. When we think about how fruit was originally available in nature, it’s a seasonal treat and wasn’t available all year round, and didn’t form such a mainstay of our diet. In Chinese Medicine it’s used sparingly and it’s used medicinally: for example, we might use pears when someone has a dry cough, which gives us the indication that maybe you wouldn’t use pears, and certain fruits, when someone has too much fluids or inflammation going on in their body because they can be moistening. It’s really interesting to consider also that the various bacteria that live within and on us can actually change our cravings – so they can actually make us crave sugar if they perceive that their fuel source is running dry and they’re starting to die out. They can change our taste buds, they can also change the level of feel-good neurotransmitters, like dopamine and serotonin – they can reward us with feel-good chemicals for eating those foods that keep them alive. So if initially it’s a little bit challenging dropping your sugar content, just bear that in mind and stick with it – it does get easier with time!
Another simple thing we can do to look after our digestive fire is not to guzzle lots of water at meal times, because it’s going to dilute that stomach acid, and the enzymes and intrinsic factor – all of those essential chemicals that our stomach is releasing in order to help us digest. Keeping a small window either side of meal times is going to help you pack the most digestive punch! Another thing you can do for yourself at meal times is to take time away from distractions – from stress, from work, from heightened emotions. Just taking time, and allowing your body that time to eat and focus on eating. In order to support that process, you might take some deep belly breaths before, during and after eating. You might take some time to feel gratitude for the food that you’re about to receive, and the people that put in the love and care to bring that food to the table. We’ve talked a bit in past episodes about the importance of the “rest and digest” nervous system (the parasympathetic nervous system) and its complimentary other half, the sympathetic nervous system (“fight or flight” system). Really, the name says it all! When we are distracted, or stressed or pressured, our body diverts resources away from the “rest and digest” system into the “fight and flight” system – the system that primes us for action. But by slowing down, by feeling grateful thoughts, and by taking slow, deep breaths, this sends a message of safety to our system, letting it know that it’s safe to slow down – to receive nutrition and to divert its energies towards the full processing, assimilation and breakdown of that nutrition.
Taking that a step further, between meals you can also take time to lie down with your hands on your belly and allow yourself time for some deep belly breaths. Very often when we’re rushing through the day, we might fall into a default pattern of shallow breathing – which again triggers that sympathetic nervous system or that “fight or flight” mode. Taking time for deep breaths allows more circulation to those digestive organs, and allows the body to fully receive the goodness that you’ve eaten. You might want to soften into the muscles of the belly – you can even put a heat pack on your belly, or even do a gentle clockwise massage over the belly.
Finally, there are a few acupuncture points that you can use. There’s a great one on the leg called Stomach 36 – I’ve included a picture of that in my show notes.
One final note is bitter flavors! Bitter flavors are an essential part of good health – and good digestive health – and they feature pretty strongly in Chinese herbal medicine. For those of you who’ve had Chinese herbs, you’ve probably had the joy of experiencing the bitter flavor!! Bitter flavors are so important because they stimulate bile production, and bile not only helps us with efficient digestion and breaking down of fats, but is also a potent antioxidant. It’s a strong alkaline substance, so it can counteract acidity in the body, and also mop up any free radicals (cells that have gone rogue, basically!) Unfortunately, our taste buds have evolved towards strong, sweet flavors, and salty and so on. They’ve evolved away from this bitter flavor, but it’s so essential and we can see how important it is in things like a lot of the classic European bitters – like Campari (my personal favorite, which has citrus and other herbs to help digestion), and also Angostura bitters, which is often added to cocktails and is a strong bitters. Things like coffee and tea, bitter greens (like broccoli, rocket, radicchio, chicory) and citrus peels as well. We use citrus peel as a medicinal in Chinese herbal medicine! So definitely incorporating some bitter flavors in your diet will supercharge your digestion.
I hope that’s been helpful and timely, and I hope it’s helping you digest all of the Christmas cheer! I will be going deeper into digestive health in future episodes: we’ll be talking about things like why we love white rice instead of brown, and we’ll be talking more about gluten and the connection there -so make sure to subscribe if you’d like to be kept up to date when those episodes come out.
Links & Research
https://www.futurity.org/sugar-gut-bacteria-protein-1941482/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5385025/
https://www.pbs.org/wgbh/nova/article/sugar-keeps-good-microbes-at-bay/
https://www.scientificamerican.com/article/how-gut-bacteria-tell-their-hosts-what-to-eat/
https://www.psychologytoday.com/au/blog/mood-microbe/201905/the-shocking-source-your-cravings
http://www.huffingtonpost.com.au/entry/gut-bacteria-brain-cognit_n_7644484.html?
Racaniello, V. (2011). Gut microbes influence defense against influenza (6.9.2011).
Retrieved from http://www.virology.ws/2011/09/06/gut-microbes-influence-defense-against-influenza/
Hollister, E. B. et al. (2015). Structure and function of the healthy pre-adolescent pediatric gut microbiome. Microbiome, 3(36).
Velasquez-Manoff, M. (2015). Gut Microbiome: The Peacekeepers. Nature, Vol. 518, Issue s7540, pS3-S11.
Velasquez-Manoff, M. (2015). How the Western Diet Has Derailed Our Evolution. Nautilus, Issue 030 (2). Retrieved from http://nautil.us/issue/30/identity/how-the-western-diet-has-derailed-our-evolution
Blaser, M. J., Chen, Y. & Reibman, J. (2008). Does Helicobacter pylori protect against asthma and allergy? Gut, Vol. 57, Issue 5, pp.561-567
Jin, X., Chen, Y. P., Chen, S. H. & Xiang, Z. (2013). Association between Helicobacter Pylori Infection and Ulcerative Colitis – A Case Control Study from China. International Journal of Medical Sciences, Vol. 10 (11). Pp.1479-1484
The Microbiome and Disease. Retrieved from http://learn.genetics.utah.edu/content/microbiome/disease/
Pollan, M. (2013). Some of My Best Friends Are Germs. New York Times, 15.5.2103) Retrieved from http://www.nytimes.com/2013/05/19/magazine/say-hello-to-the-100-trillion-bacteria-that-make-up-your-microbiome.html
Mole, B. (2016). Mounting data suggest antibacterial soaps do more harm than good. Ars, (10.4.2016). Retrieved from http://arstechnica.com/science/2016/04/mounting-data-suggest-antibacterial-soaps-do-more-harm-than-good/
Molloy, A. (2015). Mothers facing C-sections look to vaginal ‘seeding’ to boost their babies’ health. The Guardian, (18.8.2015) Retrieved from http://www.theguardian.com/lifeandstyle/2015/aug/17/vaginal-seeding-c-section-babies-microbiome
Neu, J. & Rushing, J. (2011). Cesarean versus Vaginal Delivery: Long term infant outcomes and the Hygiene Hypothesis. Clinics in Perinatology, Vol. 38 (2), pp. 321-331
Li, Q. Q., Shi, G. X., Xu, Q., Wang, J., Liu, C. Z. & Wang, L. P. (2013). Acupuncture Effect and Central Autonomic Regulation. Evidence-Based Complementary and Alternative Medicine, Vol. 2013. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3677642/
Villas-Boas, J. D., Dias, D. P. M., Trigo, P. I., Almeida, N. A., Almeida, F. Q. & Medeiros, M. A. (2015). Acupuncture Affects Autonomic and Endocrine but Not Behavioural Responses Induced by Startle in Horses. Evidence-Based Complementary and Alternative Medicine, Vol. 2015. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4568046/
Xu, Z. T., Li, R. F.., Zhu, C. L. & Li, M. Y. (2013). Effect of acupuncture treatment for weight loss on gut flora in patients with simple obesity. Acupuncture in Medicine, Vol. 31, No. 1, pp. 116-117
Li, H. K., Zhou, M. M., Zhao, A. H. & Jia, W. (2009). Traditional Chinese Medicine: Balancing the Gut Ecosystem. Phytotherapy Research, Vol. 23, pp. 1332-1335.
Alcock, Joe, Carlo C Maley, and C Athena Aktipis. “Is Eating Behavior Manipulated by the Gastrointestinal Microbiota? Evolutionary Pressures and Potential Mechanisms.” Bioessays 36, no. 10 (October 2014): 940–49.
Behary, Preeshila, and Alexander D. Miras. “Food Preferences and Underlying Mechanisms after Bariatric Surgery.” The Proceedings of the Nutrition Society 74, no. 4 (November 2015): 419–25.
Goncalves-Leitao R, Carvalho-Santos Z, Francisco AP, Fioreze GT, Anios M, Baltazar C, Elias AP, Itskov PM, Piper MDW, Ribeiro C (2017) Commensal Bacteria and Essential Amino Acids Control Food Choice Behavior and Reproduction. Plos Biology 15(4)
Temko, Jamie E., Sofia Bouhlal, Mehdi Farokhnia, Mary R. Lee, John F. Cryan, and Lorenzo Leggio. “The Microbiota, the Gut and the Brain in Eating and Alcohol Use Disorders: A ‘Ménage à Trois’?” Alcohol and Alcoholism 52, no. 4 (July 1, 2017): 403–13.
More on Dr. Maz
balancedacupuncture.com.au
www.instagram.com/balanced_with_drmaz/
www.facebook.com/balancedwithdrmaz
Disclaimer
Chinese Medicine is a personalised, functional medicine that treats the individual and the root cause of their presenting imbalance (what conventional medicine would call the symptom, disease or condition). This means that your doctor of Chinese Medicine will work one-on-one with you to achieve a personalised treatment plan. As such, this podcast is for informational purposes and is not intended to diagnose, prescribe or substitute existing medical advice.
© Copyright Balanced Acupuncture & Chinese Medicine and Dr. Maz Roginski 2020
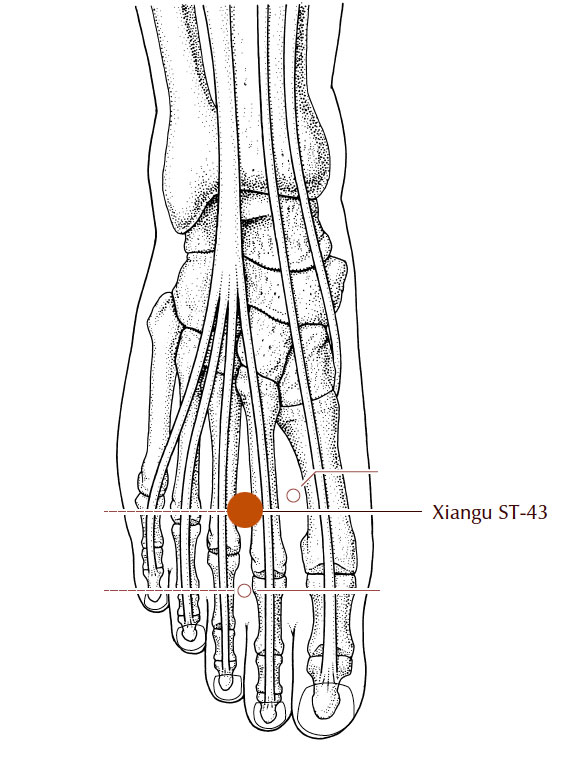
Stomach 43
image: A Manual of Acupuncture, Deadman & Al-Khafaji
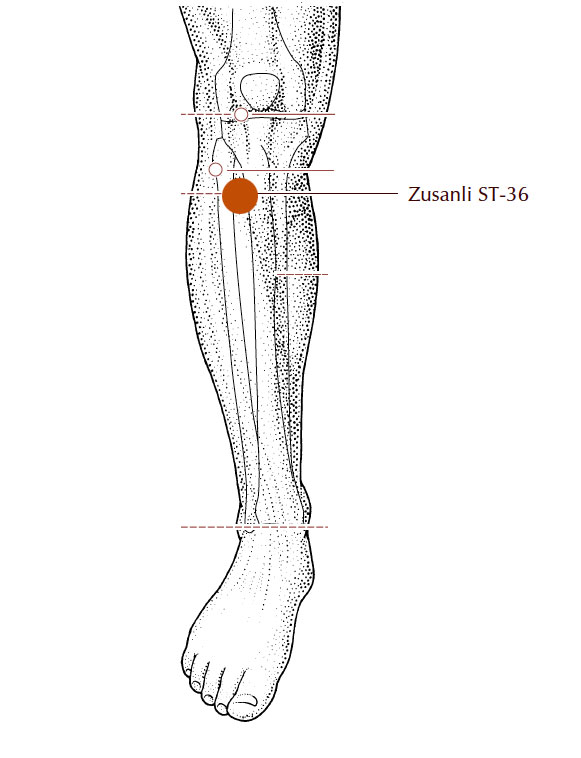
Stomach 36
image: A Manual of Acupuncture, Deadman & Al-Khafaji
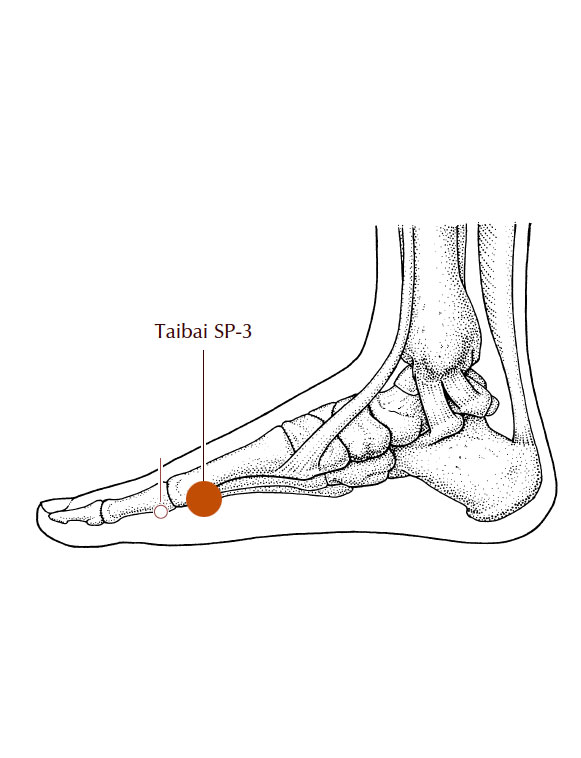
Spleen 3
image: A Manual of Acupuncture, Deadman & Al-Khafaji

Like the rest of this podcast series, I found the explanation and logic of how of how the Chinese approach to maintaining health, (so much of a mystery to most of us), to actually complement the contemporary science findings of Western medicine. Includes some useful general tips we could all derive some benefits from.
I look forward to further episodes
Thank you so much for your feedback, Ian – I’m so happy to hear you enjoyed it and found it complementary to Western medicine findings too.
Thanks for your personal marvelous posting! I actually enjoyed reading it,
you could be a great author. I will remember to bookmark your
blog and will eventually come back later in life. I
want to encourage continue your great writing, have a nice morning!